The severity of Covid-19 on the human body can vary significantly. In some patients, this virus will cause no symptoms while in others, the symptoms could be life-threatening. It is also true that some people are more susceptible to COVID than others.
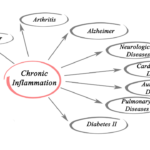
At the same time, a common denominator of COVID infections seems to include inflammation in the body. Having chronic inflammation already for various reasons such as overweight or type 2 diabetes are among the undesirable risk factors for a bad bout with COVID-19.
And then, the infection itself triggers inflammation in various important parts of the body.
A more classical understanding of inflammation is that it occurs after an acute injury. The main ways it develops include swelling, redness, heat, pain, and loss of function of the injured part.
Covid is more serious and prevalent among men and the elderly population, especially those suffering from other health conditions such as obesity and diabetes. In most Western countries, ethnic minority communities are also disproportionately affected.
While there are numerous factors contributing to COVID infections and its severity, such as occupational exposure, lack of access to proper healthcare, and environmental hazards such as pollution, research shows that for some of the groups that are more susceptible to the virus, it is their immune system’s response that explains why they get so sick.
Researchers have come to the conclusion that risks associated with conditions such as obesity, sex. diabetes, and age are all linked to the irregular response of the immune system when confronted by COVID.
How Far Can Inflammation Go?
One of the common symptoms observed in individuals with serious COVID is severe lung damage due to extremely vigorous immune response. The condition is characterized by the release of numerous inflammatory mediators known as cytokines.
You will also hear people call this the “cytokine storm.”
Cytokines are highly powerful immune response tools: they can actually slow or maybe stop virus reproduction.
However, some other functions of cytokines such as the regeneration of other cells to assist battling the infection or the enhancement of the ability of the already recruited immune cells to get across your body’s blood vessels can cause severe damage if not properly controlled. That’s exactly what happens during a cytokine storm.
The cytokines and the associated storms are created by the defensive immune system of the body — including white blood cells, macrophage cells, and monocyte cells. When under proper control, these cells form the force required by your body’s immune system to fight against illnesses, repair damaged body tissues, and recruit more immune cells for backup.
However, when one is suffering from severe COVID, the way macrophage cells and monocyte cells work misfires. This is especially true in individuals with obesity and diabetes.
What Role Does Glucose Play?
High blood levels of glucose might fuel damage. If not effectively controlled, diabetes could lead to extremely high glucose levels in a patient’s body. According to a recent study, monocytes and macrophages in COVID positive patients respond to high glucose levels with life-threatening consequences.
SARS-CoV-2, the virus responsible for causing COVID, requires a target to bolt onto for it to invade the body cells. The virus chooses the ACE2 receptor, which is a protein on the cell surface.
High glucose levels in the body raise the amount of ACE2 on monocytes and macrophages, aiding the virus to attack the same cells that are supposed to kill it.
Once the virus has infected the monocytes and macrophages, it causes these cells to produce high levels of inflammatory cytokines, triggering the cytokine storm. By now, you can tell that the higher the glucose levels in your body, the more effective the virus gets in replicating inside your immune cells. In other words, glucose fuels the COVID virus.
The virus does not stop at that. It further causes the already virally infected cells to produce products that damage the lungs, like reactive oxygen species. Due to this, other immune cells such as lymphocytes are rendered weak and incapable of killing the virus.
It is also important to note that obesity also leads to high glucose levels, the same way that diabetes does, affecting monocyte and macrophage activation. Research also shows that macrophages in obese people are a favorite place for the SARS-CoV-2 virus to thrive.
Other Risks Related To Inflammation
The inflammations observed in individuals with obesity and diabetes is also seen on the elderly population (from 60 years and above). This can be explained as a phenomenon called infammageing.
The major characteristic of inflammageing is high pro-inflammatory cytokines levels. This could be caused by various factors among them being obesity, genetics, and microbiomes such as viruses, bacteria and other microbes living inside your body.
Most of the people grouped as the elderly have fewer effective lymphocyte cells, the cells that could help kill the virus. This means that for some older folks, the immune system is not only too weak to fight the virus, but it’s also likely to damage their ability to respond to external invaders like viruses.
Vaccines many also not function effectively with low lymphocytes levels. This is very critical when making any plans for future COVID-19 vaccine campaigns
Another worrying puzzle that researchers have been trying to crack is why men are more vulnerable to COVID. Studies show that immune cells in men are more susceptible to SARS-CoV-2 as compared to those in women. The ACE2 receptors that the SARS-CoV-2 latches onto are more plentiful in men than in women.
There are also higher levels of TMPRSS2 enzymes in men. These enzymes promote the ability of COVID virus to enter body cells.
Immunology also tries to shed some light on the justification of the sex differences. The fact that women and men differ in immune response has existed for ages, and the same is true for COVID.
A different study tracked and compared immune responses to SARS-CoV-2 virus in women and men. The results showed that men are more susceptible to the development of atypical monocyte cells that are pro-inflammatory and possible of triggering a cytokine storm.
Women, on the other hand, were observed to have a T cell response system which is necessary for effective killing of the virus. However, advancement in age and having huge body masses reversed the strong immune response in women.
These studies show how different our bodies are and that the more we comprehend these vulnerabilities and differences, the more effective the treatment approach will be. With this data, it is important to consider the variations in immune responses and include individuals from varying demographics in vaccine and drug trials.
Foods That Fight Inflammation
Some diets have ingredients that might worsen or trigger inflammations. Processed and sugary foods are more likely to do this while whole and fresh foods are less likely to cause these effects.
Most anti-inflammatory diets focus on vegetables and fruits. Most plant-based foods are great sources of antioxidants. However, other foods can also trigger the production of free radicals. Examples of foods likely to cause the production of free radicals are foods fried in repeatedly heated cooking oil.
Taking foods with dietary antioxidants helps in removing free radicals from your body. These free radicals are by-products of some of our body processes such as metabolism. However, external circumstances such as smoking and stress could increase the levels of free radicals in the body.
Free radicals cause cell damage, and this damage raises the risk of inflammations which subsequently lead to a number of diseases. Our bodies naturally produce antioxidants that help with the removal of the free radicals, but dietary antioxidants could also help.
A good anti-inflammatory diet is one that contains foods rich in antioxidants. Omega-3 fatty acids, for example, helps with the reduction of inflammatory-proteins in your body. According to The Arthritis Foundation, fiber could also have the same effect.
Various Forms of Anti-Inflammatory Diets
Some of the popular diets have anti-inflammatory principles. For instance, the DASH and the Mediterranean diet include vegetables, fresh fruits, whole grains, fish, and fats that are good for the heart.
Inflammations play a huge role in COVID and cardiovascular diseases, but studies show that the Mediterranean diet, with the focus on healthful oils and plant-based foods, could lower the effects significantly.
Who Can Benefit?
You can integrate an anti-inflammatory diet into your therapy program for conditions that worsen with chronic inflammations. Some of these conditions are:
- rheumatoid arthritis
- asthma
- psoriasis
- eosinophilic esophagitis
- colitis
- Crohn’s disease
- inflammatory bowel disease
- Hashimoto’s thyroiditis
- lupus
- metabolic syndrome
Metabolic syndrome is a collection of conditions that occur simultaneously, and among them being obesity, type 2 diabetes, cardiovascular disease, and high blood pressure.
Research shows that inflammation plays a role in all of them. Feeding on an anti-inflammatory diet could, therefore significantly improve the health of people with metabolic syndrome. Eating foods rich in antioxidants will also reduce the risk of COVID and certain cancers.
Food To Eat
A healthy anti-inflammatory diet should contain a combination of various foods that offer a range of antioxidants, are rich in nutrients and contain healthful fats.
Some of the foods that fight inflammation include:
- oily fish, such as salmon and tuna
- fruits, such as strawberries, cherries, blueberries, and blackberries,
- vegetables, including broccoli, kale, and spinach
- beans
- olives and olive oil
- nuts and seeds
- fiber
Other recommendations include the following:
- moderately cooked or raw vegetables
- legumes, such as lentils
- spices, such as turmeric and ginger
- prebiotics and probiotics
- some herbs
- tea
It is also worth remembering that:
A single food cannot boost your health. It is vital that you include other healthy ingredients in your diet.
Simple, fresh vegetables are the best. Proceed, foods have their nutritional content changed during the process.
You should always check the labels of all pre-made foods before buying. For instance, cocoa is good for your health, but most cocoa products contain fat and sugars.
It is important to vary the colors of your foods, vegetables, and fruits as this increases the range of antioxidants and nutrients.
Foods That You Should Avoid
When following an anti-inflammatory diet, you should limit or avoid the intake of:
- Unhealthy oils
- Processed foods
- Excess alcohol
- Processed snacks such as crackers and chips
- Processed carbs such as white pasts, white bread, and other baked products
- Premade desserts like candy, ice cream, and cookies
Additionally, you should limit your intake of:
Gluten: Some individuals experience inflammatory-reactions after taking gluten. Gluten-free diets are restrictive and not suitable for everyone. Once you realize that gluten is triggering specific symptoms, you should consider taking to a gluten-free diet.
Nightshades: Plants in the nightshade grouping such as eggplants, potatoes, tomatoes, and peppers can trigger flares in some individuals prone to inflammation. You can try reducing nightshades to 2-3 times a week and observe whether the symptoms will disappear.
Be aware that tobacco itself is a nightshade plant.
Carbohydrates: Studies show that high carb intake can cause inflammation in some individuals, even though some carbohydrates are healthy. More complex such as whole grains and sweet potatoes, are rich in nutrients and antioxidants.
Will a Vegetarian Diet Work?
This can be an option. People following a vegetarian diet have lower inflammatory makers. Eating animal foods increases the risk of insulin resistance and systematic inflammations. But you need some good sources of quality proteins, e.g., fatty fish like salmon that give you the antiinflammatory omega-3 fatty acids.
Anti-inflammatory Diet Tips
You might find it challenging to transition to a new diet, but these tips might be of great help.
- Buy a variety of vegetables, healthy snacks, and fruits weekly
- Gradually substitute fast foods with homemade healthful meals
- Replace sugary drinks such as soda with sparkling or still mineral water.
- Consult a healthcare professional about healthy supplements such as multivitamins and cod liver oil.
- Always sleep enough.
- Exercise for at least 30 minutes a day
Summary
Inflammation can increase our risk or worsen COVID infections. To help avoid these effects, it is important that you consider switching to an anti-inflammatory diet.
However, there is no single anti-inflammatory diet that will cover it all; instead, the diet should include lots of vegetables, fresh fruits, healthful fats, and whole grains. If you suspect that you may have an inflammation problem, you should seek the attention of a medical professional and work on improving your diet.
Finally, be aware that some anti-inflammatory supplements from food sources may also be helpful in combatting the worst inflammatory responses to a COVID infection. Talk to your doctor about quercetin, for example, which can stabilize mast cells, a major cell involved in allergies and histamine release in inflammation.